IMPORTANCE:
Following animal model data indicating the possible rejuvenating effects of blood from young donors, there have been at least 2 observational studies conducted with humans that have investigated whether donor age affects patient outcomes. Results, however, have been conflicting.1
OBJECTIVE:
To study the association of donor age and sex with survival of patients receiving transfusions.
DESIGN, SETTING, AND PARTICIPANTS:
A retrospective cohort study based on the Scandinavian Donations and Transfusions database, with nationwide data, was conducted for all patients from Sweden and Denmark who received at least 1 red blood cell transfusion of autologous blood or blood from unknown donors between January 1, 2003, and December 31, 2012. Patients were followed up from the first transfusion until death, emigration, or end of follow-up. Data analysis was performed from September 15 to November 15, 2016.
EXPOSURES:
The number of transfusions from blood donors of different age and sex. Exposure was treated time dependently throughout follow-up.
MAIN OUTCOMES AND MEASURES:
Hazard ratios (HRs) for death and adjusted cumulative mortality differences, both estimated using Cox proportional hazards regression.
RESULTS:
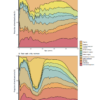
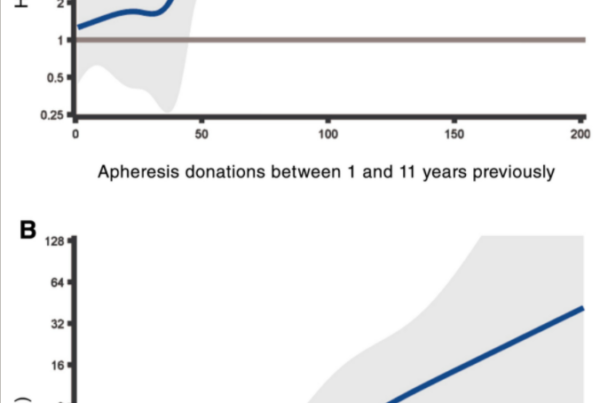
Results of a crude analysis including 968 264 transfusion recipients (550 257 women and 418 007 men; median age at first transfusion, 73.0 years [interquartile range, 59.8-82.4 years]) showed a U-shaped association between age of the blood donor and recipient mortality, with a nadir in recipients for the most common donor age group (40-49 years) and significant and increasing HRs among recipients of blood from donors of successively more extreme age groups (<20 years: HR, 1.12; 95% CI, 1.10-1.14; ≥70 years: HR, 1.25; 95% CI, 1.08-1.44). Higher mortality was also noted among recipients of blood from female donors (HR, 1.07; 95% CI, 1.07-1.07). Adjustments for number of transfusions with a linear term attenuated the associations, but the increased mortality for recipients of blood from young, old, and female donors was not eliminated. Closer examination of the association between number of transfusions and mortality revealed a nonlinear pattern. After adjustments to accommodate nonlinearity, donor age and sex were no longer associated with patient mortality.
CONCLUSIONS AND RELEVANCE:
Donor age and sex were not associated with patient survival and need not be considered in blood allocation. Any comparison between common and less common categories of transfusions will inevitably be confounded by the number of transfusions, which drives the probability of receiving the less common blood components. Previous positive findings regarding donor age and sex are most likely explained by residual confounding.